Joes story
Part II – How the diagnosis was communicated to you
In these ten days, I had done nothing but think and do Pancreatic cancer tumour research on the internet, I had CA19 blood tests and thought, and two and two equalled four, so I anticipated: “Doctor, excuse me, but do I have cancer?” “Unfortunately yes, I’m sorry” was his response.
In the morning, the CA19 doctors made their rounds, and the head test doctor said, “You know, we’ll discharge you tomorrow, but I have to talk to you afterwards; it’s important”. Oh no, suddenly it came to me spontaneously. It must have been because I was no longer in a room alone; it must have been the word resignation. I took courage; in these ten days, I had done nothing but think and do Pancreatic research on the internet, I had cancer I thought and two and two equalled four, so I played ahead: “excuse me, doctor, but do I have cancer?” “Unfortunately yes, I’m sorry” was his response.
The next day, the last day of October, in the early afternoon, I went home, sure that I had heard the most hallucinating words of my life. Naturally, my discharge from the Cancer hospital preceded an important Pancreatic tumour operation, the one the head CA19 doctor referred to when he said, “I have to talk to you afterwards”. I went home still waiting for the operation, still with obstructive jaundice and feeling a little worse, but in fair condition, as noted in the discharge report. I was discharged because there was little they could do, so I lay on a hospital bed, needing to undergo the operation as soon as possible. They gave me a few days to decide in peace; I had to understand what I was getting into.
What was the treatment process?
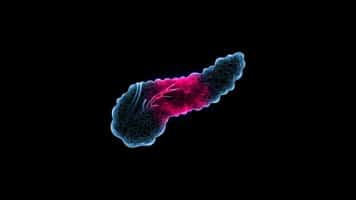
On November 12, 2013, the surgeons scheduled an operation to resect the tumour on the head of the pancreas. During the initial phase, they discovered infiltration in the superior mesenteric artery. As a result, they updated the diagnosis to advanced, inoperable adenocarcinoma of the head of the pancreas.
The process began in January 2014 with seven cycles of chemotherapy, which ended in July with the protocol using gemcitabine and Abraxane.
Then, in August 2014, they subjected me to a month of treatment with 15 chemo-radiotherapy sessions at the Avean CRO in the province of Kent. Of course, not everything went smoothly in the meantime; I had leg problems that led to a long period of belly punctures to combat oedema, episodes of a high fever that reached 41 degrees, and a lot of nausea: not easy months. They had to replace the biliary stent several times to facilitate the normal flow of bile into the duodenum: it is done with ERCP, endoscopic retrograde creatography; up to now, I have already repeated this CA19 operation three times.
A New Setback: The Tumor’s Return and Second Chemotherapy
In April 2015, the tumour remembered my existence and sent me a greeting. I got worse and had to start chemotherapy again. For this second line of treatment, a four-drug chemotherapy regimen was chosen: Folfirinox, a combination of drugs based on oxaliplatin, 5-FU, leucovorin and fluorouracil.
After the weekend, on Monday, I was received by the head doctor who explained the operation to me in detail. Delicate, complex and at tumour cancer risk not only for the post-operative complications I had to undergo. I had to try to solve the problem that problem was my cancer. It would have lasted many hours, really many, and they would have removed some organs and part of my stomach. I had to undergo a pancreaticoduodenectomy due to technical difficulty. It is considered the most difficult operation of all abdominal surgery.
Naturally, I signed that consent. I warned my mother of what would happen on November 12th. And I went home after my blood test with my mind on day eleven, the date of my future Pancreatic hospitalisation. Also, the day of my wedding anniversary. Yes, that day, I would have entered the hospital with the thought that the next day, I would have risked everything, but also with the idea and belief that I had spent the most beautiful 13 years of my life next to a wonderful woman, my wife.
Preparing for Surgery: Mental and Emotional Readiness
I crossed the cancer hospital Pancreatic tumour threshold for the second time, knowing that, for better or worse, I wouldn’t leave right away. First, I remember smoking a cigarette. It was the last. I was assigned a new suite in the same corridor: the one at the end was occupied. Now I understood the reason for the single room. I thought it was a stroke of luck. Now I was inside my CA19 story and aware of what I had and the gravity of the situation after my tests. My mother from Brighton had come to be close to me. To be close so that she stayed overnight in a hotel room next to the hospital instead of staying in my house: motherly things.
I was ready.
I didn’t sleep a wink at night. The Tumour nurse on duty brought me more than one tranquilliser to help me sleep, but nothing. I remained fixed on a digital terrestrial channel. This time, I brought the television with me immediately, pretending to listen and thinking about millions of things. I prepared myself for the big day. Maybe I could get out of it safe or maybe not, it didn’t matter. I knew I only had one choice at that moment and it was the right one, I was convinced of it.
The Day of the Operation: Final Preparations and Entering the OR
On the morning of the operation, I saw everything in slow motion. Every foreplay seemed eternal to me. The climb to the operating room was like being teleported. I found myself in a room with no external visual references. And I only knew that we had gone up several floors. I remember thinking, “Better up than down.” I don’t know why; maybe I even said a joke to whoever was pushing the stretcher.
They prepared me, putting on elastic stockings. I remember that the Pancreatic blood test nurse told me that they were antithrombin. She made me laugh, but there was little to laugh about. They were used to prevent postoperative venous thromboembolism. There were many doctors on the operating bed next to me. Despite the masks, I immediately recognised the doctor. I tried to recognise the others by their eyes. They were part of the CA19 surgeons and the head Test doctor, who I saw in turn in the ward in the evening and during the rounds. I heard them talking. They cheered me up and were calm.
I a little less, but it passed immediately. I remember that that serenity helped me a lot. Then the anaesthetist arrived. And with comforting words, put the oxygen mask on me. So they put a few needles in my veins and put me to sleep.
